|
|
АкушерствоАнатомияАнестезиологияВакцинопрофилактикаВалеологияВетеринарияГигиенаЗаболеванияИммунологияКардиологияНеврологияНефрологияОнкологияОториноларингологияОфтальмологияПаразитологияПедиатрияПервая помощьПсихиатрияПульмонологияРеанимацияРевматологияСтоматологияТерапияТоксикологияТравматологияУрологияФармакологияФармацевтикаФизиотерапияФтизиатрияХирургияЭндокринологияЭпидемиология |
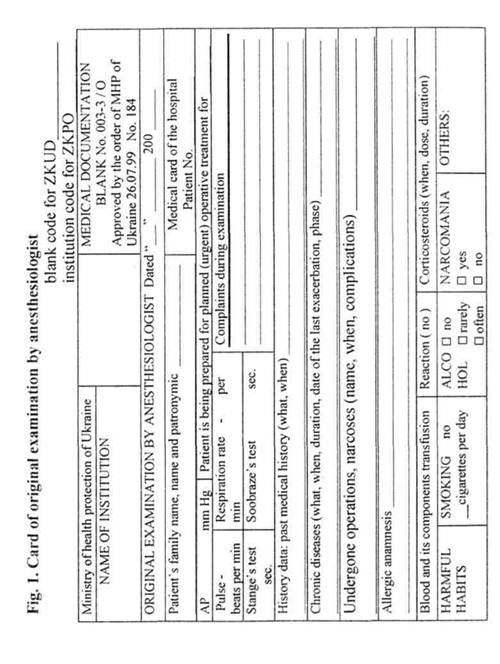
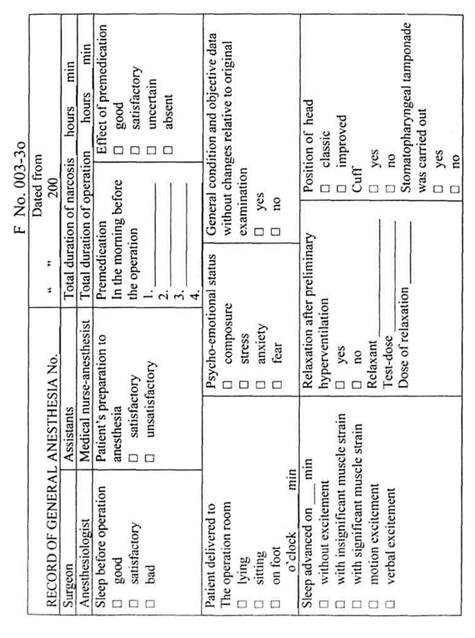
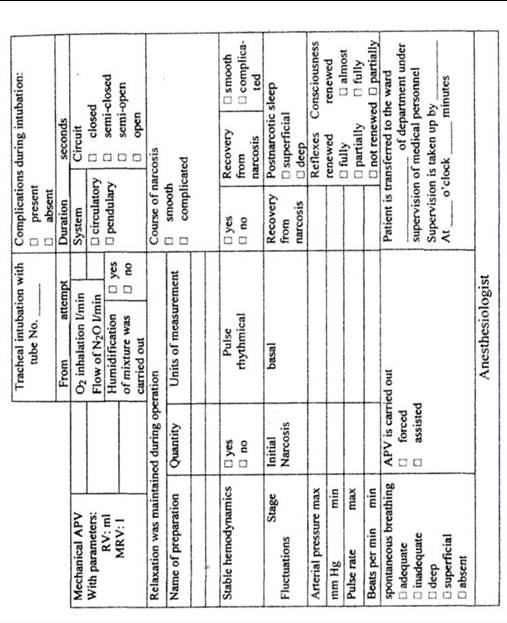
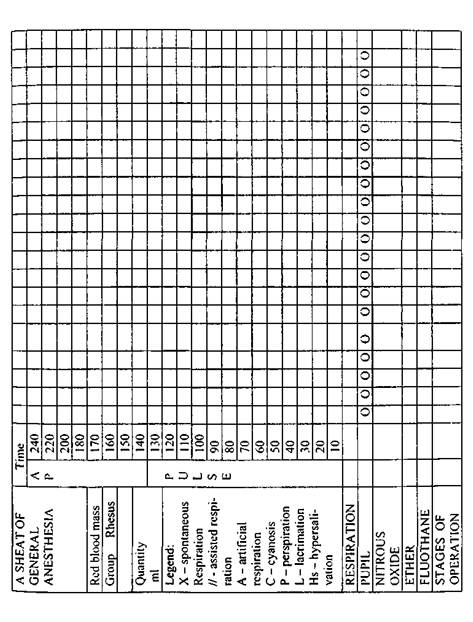
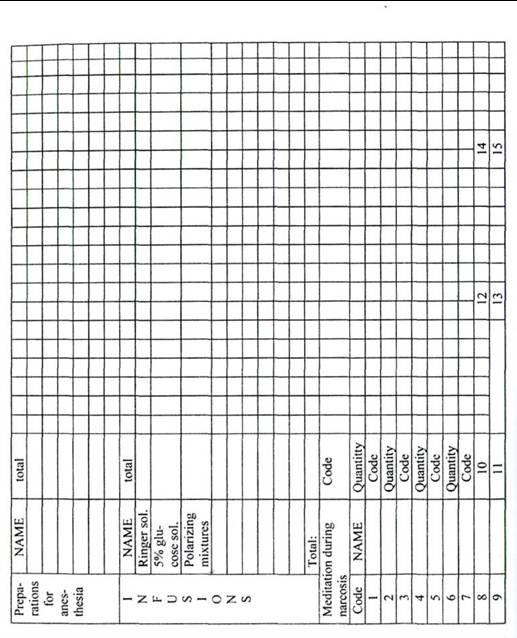
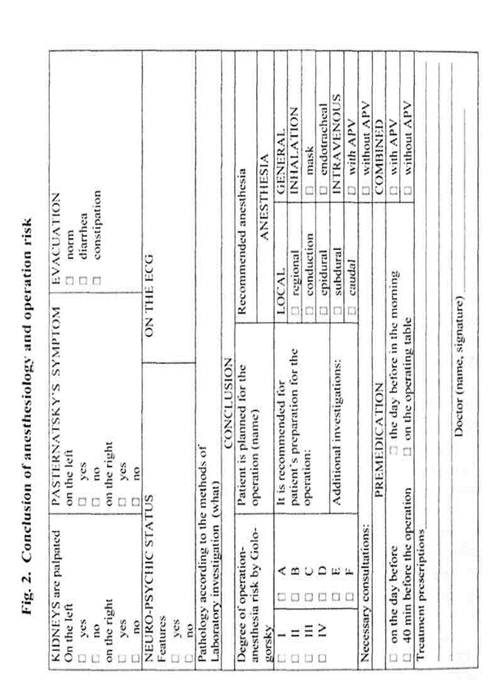
MYORELAXANTSIn order to understand a mechanism of myorelaxants action, it is necessary to examine, briefly, the arrangement and functioning of neuromuscular synapse. It consists of presynaptic part, synaptic slit and postsynaptic membrane (end plate), representing a component part of plasmalemma of muscular fiber, having H-cholinoreceptors. The action of neuromuscular synapse can be described, in brief, as follows: motor impulse coming along a motor neuron sharply increases Ca++ concentration in the nerve ending, as a result, synaptic vesicles, being here, release acetylcholine into a synaptic slit. The released acetylcholine is being bound with H-cholinoreceptors of the end plate, opening, for a short time (1 msec), the canals through which Na++ and Ca++ ions enter the inside of muscular fiber, and K+comes out. Polarization of membrane takes place, and the action potential arises that is spreaded along the whole muscular fiber triggering the process of its contraction. While the acetylcholine-H-cholinoreceptor complex is disintegrated, a postsynaptic membrane is repolarized. Acetylcholine is destroyed by acetylcholinesterase, and choline, so formed, returns to the presynaptic ending for a replenishment of the acetylcholine supplies in the synaptic vesicles. By their mechanism of action myorelaxants are divided into depolarizing and nondepolarizing. Depolarizing myorelaxants (dithylinum, myorelaxine, lysthenon) represent themselves a double acetylcholine molecule. Binding with postsynaptic H-cholinoreceptors, they cause a depolarization of the end plate. But as long as depolarizing myorelaxants, unlike acetylcholine, practically are not destroyed by acetylcholinesterase, a depolarization proves to be stable that leads to nonexcitement of the membrane of muscular fiber, adjacent to synapse, and comes a muscular relaxation. A depolarizing block is being finished when myorelaxant is eliminated from synapse into the blood, where it is quickly destroyed by pseudocholinesterase, at first — down to choline and succinyl-monocholine, and then succinyl-monocholine (preserving 1/20 of myoparalytic activity) is converted much slower into end products — choline and succinic acid. Side effect of depolarizing myorelaxants lies in the appearance of muscle pains after their application (owing to myofibrillation observed in the initial phase of action), increase of AP, HR (stimulation of sympathetic ganglia and adrenals with high doses of myorelaxants), bradycardia (prevented by atropine administration), increase of K+ level in plasma by 0.5-1 mmol/1, that may cause a dangerous hyperkaliemia and disorder of cardiac activity in burns, extensive traumas and prolonged adynamia in bed, increase of intraocular pressure, intraventricular pressure in muscular fasciculations, a moderate short-term elevation of cerebral blood flow and ICP. After a long use of high doses of depolarizing myorelaxants a repeated myorelaxation (the socalled double block or recurarization) may be observed, the mechanism of which is unclear (possibly, accumulation of acetylcholine acting as a depolarizing myorelaxant). A prolonged blockade (protracted apnea) may be due to the insufficiency (late terms of pregnancy, diseases of the liver, starvation, anemia, carcinoma, burns, shock, uremia, heart failure, radiation therapy) or medicamentous inhibition of pseudocholinesterase activity in plasma (anticholinesterase preparations, for example, eye drops, MAO inhibitors, some local anesthetics, poisonings with organophosphorus compounds and others), as well as its genetic defects. Nond epolarizing myorelaxants, because of th eir high affinity to postsynaptic cholinoreceptors, compete with acetylcholine for these receptors and impede its depolarizing effect. Because of the duration of their action, nondepolarizing preparations are called myorelaxants of long-term effect, though some of them (mivacurium) are quickly hydrolyzed by cholinesterase and referred to myorelaxants of short-term effect. As for side effects one should mark the ability of some myorelaxants (d-tubocurarine, metocurin, atracurii besilas, mivacurium) to cause arterial hypotension as a result of histamine release that is prevented by a slow administration of preparations and preliminary prescription of antihistaminic agents. A discontinuation of neuromuscular nondepolarizing block occurs to the extent of myorelaxant evacuation from the synapses. Acceleration of this process may be achieved by prescription of anticholinesterase agents contributing to acetylcholine accumulation in a synaptic slit, competitively forcing out myorelaxant: edrophonia (tensilon), proserinum (neostigmine) and pyridostigmine (kalymin). In so doing, atropine is introduced to prevent M-cholinergic stimulation with hypersalivation, bradycardia, lacrimation, myosis, bronchospasm. Duration of this blockade is under the influence of a number of other factors — features of the applied myorelaxant and its dose, a deepness of narcosis, presence of electrolyte disturbances, ABB shifts, hypothermia, a use of some antibiotics and other medicinal agents, as well as a number of associated diseases. A grave pseudoparalytic myasthenia (myasthenia gravis), Itton-Lamberg's myasthenic syndrome accompanying oncologic diseases, muscular dystrophies (muscular Duchenne's dystrophy et al.) require timely revelation before the operation, correction treatment and preparedness for a prolonged ALV. Thus, an up-to-date anesthesiologic provision is considered as a set of components, a carrying out of which is possible by means of mononarcosis with conventional anesthetics, but it is more expedient and safe to use special neurotropic agent, in order to achieve each component. A procedure of anesthesiologic provision of operative interventions includes several stages, starting from the moment of taking a decision by the surgeons to perform the operation and finishing with the postoperative period. Anesthesiologist's participation in patient's management starts with an acquaintance with medical history and a patient himself, his additional examination by anethesiologist, in order to detect and correct those deviations in the patient's organism, that could influence a safety in the course of anesthesia, operation and postoperative period. Anesthesiologist, acquainted with the data of medical history, begins questioning the patient: finds out an occupational anamnesis and influence of production process on his health, childhood diseases, past operations, deliveries and reactions to anesthesia, traumas and their consequences, presence of habitual mandibular dislocation, past and chronic diseases, hereditary diseases of the patient and his close relatives, drugs taken at present, allergic reactions, harmful habits, menses and obstetric history. He clears up the time of the last water and food intake that is particularly important in urgent cases. In the time of questioning and further physical examination, anesthesiologist examines his patient paying attention to emotional state, his physical activity, features of constitution and external signs of the basic and associated diseases that may be of importance for the choice and management of anesthesia. During physical examination, height and body mass, AP, pulse, the rate, deepness and character of respiration, Stange's-Sabrazes test are determined. The head and neck are examined: opening of the mouth, examination of a pharynx with the estimation according to Mallapati (class I — palatine arches and soft palate are visible; class II — palatine arches and soft palate are visible, but uvula is hidden behind the root of the tongue; class III — only a soft palate is visible; class IV — only a hard palate is visible, a difficult intubation should be expected), the distance from the margin of the mandible to the upper edge of the thyroid cartilage (less than the width of 3-4 fingers — a difficult intubation is possible) is determined, the oral cavity and teeth are examined paying attention to the presence of removable dentures, a neck mobility is also checked. The heart and lungs are auscultated. The abdomen is examined and palpated (distention, formations, ascites, predisposing to regurgitation and respiratory failure), the extremities (muscular atrophy, "drumstick fingers", cyanosis, protruded veins, contamination of skin) are also examined. Neurologic and mental states are defined. Laboratory investigations should not be superfluous or insufficient. All examinations, except blood analysis for RW, HIV-infection, blood group and Rh factor, total blood count and urinalysis, should be substantiated by the patient's condition or planned operation. A compulsory hematocrit is recommended for infants under 6 mos., women over 50 and men over 65. A biochemical blood analysis is carried out, if specific clinical indications are available. ECG is indicated for males over 40 and females over 50. Chest X-ray is made according to indications, and roentgenoscopy is to be done for all! Findings of the examination are recorded in the card of the primary examination of anesthesiologist (Fig. 1) that is a medicojuridical document. Here a conclusion of anesthesiologic and operative risk is given (Fig. 2). When there are some features not stipulated by the card, a detailed record should be done in the medical history, for the most part in urgent cases. It is considered that in relations with the patient an anesthesiologist must stick to the principle of the "informed consent": the patient has a right to know about his condition all, what he is interested in, and without patient's consent it is impossible to carry out any investigation, manipulation or intervention. It means that the anesthesiologist must be, with the rare exception, perfectly frank with the patient with regard to his
diagnosis, condition, forthcoming anesthesia, expected complications. The patient and his relatives must know the average duration of similar operation, that in some specified cases the patient may wake up not in the ward, but in the intensive care department, and how long ALV may continue following the operation. The anesthesiologist may, only in general terms, describe the character of the operation, and in case of the patient's interest to the details, he should be readdressed to the surgeon. It is not recommended to discuss with the patient, as far as this operation is necessary for him (it is more a job for the surgeon) and whether the surgeon is able to perform it skillfully (as well as it is inappropriate for the surgeon to discuss with the patient the anesthesiologist's professional abilities). Anesthesiologist chooses a procedure of anesthesia, taking into account surgeon's and patient's wishes. Normal relations between the anesthesiologist and the surgeon anticipate a mutual informing of planned actions and even joint discussion of these actions, as far as they both are, in equal degree, responsible for the patient's fate, but if a conflict arises one should remember the words of one wise anesthesiologist: "that specialist must be more dominant who is cleverer". It is not excluded that to take particularly crucial decisions it would be expedient to invite senior, by their position, specialists and a representative of the administration. As for a refusal to carry out anesthesia, here, only two reasons are competent: unwillingness of the patient or technical impossibility to perform the operation. In other cases the anesthesiologist is obliged to do all to ensure a carrying out of anesthesia. In urgent situations, at present, the problem of contra-indications for narcosis is incompetent. The problem is being solved only about the form and method of anesthesia, about the patient's preparation for the operation depending on his state conditioned by basic and associated pathology. Patient's preparation for anesthesia envisages a restriction of food and water intake (as a rule "nothing per os") and premedication. Usually the patients should not take hard food 6 hrs before the operation. In a case of the operation "at risk" (obesity, pregnancy and others) drugs diminishing an acidity of gastric juice (antacids) are prescribed. In separate cases (for example, pyloric stenosis) and in urgent situations before the operation a gastric evacuation is carried out by means of gastric tube with a large lumen that is removed immediately before initial narcosis. Medicamentous preparation is intended to decrease the influence of stress associated with waiting for the operation, unfavorable side effects of anesthetics, as well as the main and associated pathology. Premedication is subdivided into preliminary and immediate.
General component of preliminary premedication is mental tranquility. To achieve this, diazepins are more often used which, unlike barbiturates of prolonged action, do not cause allergic reactions and a "hangover" syndrome. Specific component is represented by the agents aimed to treat basic and associated pathology. An immediate premedication is carried out in planned operations more often intramuscularly, more rarely per os taking a drug with a small amount of water in the ward 30 min before the patient's transportation to the operating room, and in emergencies intravenously on the operating table immediately before initial anesthesia. The tasks of such premedication are: prevention of emotional stress, neurovegetative stabilization, decrease of salivary and bronchial glands secretion, potentiation of general and local anesthetics effect, prevention of allergic reactions to the medicaments and infusion-transfusion agents administered in the process of anesthesia. These tasks are fulfilled by an individual selection of drugs with M-choli-nomimetic, analgetic, sedative and antihistaminic action (Table 4). Before proceeding to carrying out anesthesia, the doctor must make sure that the working place is ready. A list of apparatuses, equipment, instruments and medicaments necessary for the work is given below. Table 4 Method of application and doses of preparations most often used for premedication (according to L.V. Usenko et al., 1995 with supplements)
|
При использовании материала ссылка на сайт medlec.org обязательна! (1.585 сек.) |