|
|
АкушерствоАнатомияАнестезиологияВакцинопрофилактикаВалеологияВетеринарияГигиенаЗаболеванияИммунологияКардиологияНеврологияНефрологияОнкологияОториноларингологияОфтальмологияПаразитологияПедиатрияПервая помощьПсихиатрияПульмонологияРеанимацияРевматологияСтоматологияТерапияТоксикологияТравматологияУрологияФармакологияФармацевтикаФизиотерапияФтизиатрияХирургияЭндокринологияЭпидемиология |
Fig. 24. The simplest devices for artificial pulmonary ventilation: a) Safar airway; b) Ambou's bag; c) RDA-2
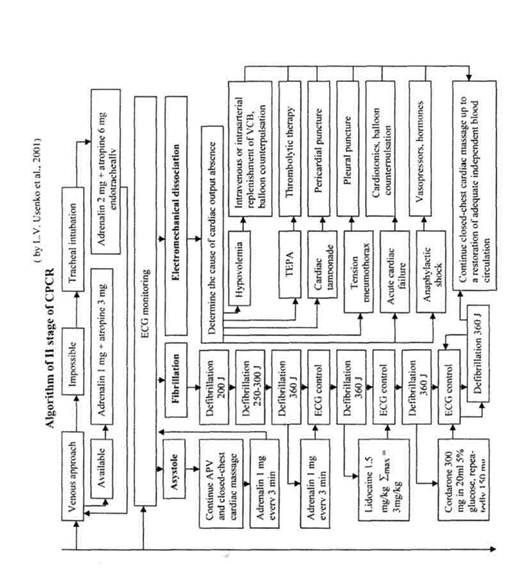
A closed-chest cardiac massage is continued, ECG is being taken, and if a macrowave fibrillation is registered on ECG, — one should proceed to an immediate defibrillation. But the main thing that is possible at the specialized stage — it is an application of medicamentous agents. That way of administration of medicaments should be selected which may be used in a maximum short time: intravenously with a preferred use of central veins (subclavian, femoral), endotracheally through an endotracheal tube or a puncture of cricothyroid ligament. An intracardiac injection, widely applied earlier, is not recommended. They start with the preparations of "primary administration" that are introduced irrespective of the cause and form of circulatory arrest. This is, first of all, adrenalin contributing to the restoration and increase of cardiac activity. Several variants of its dosage are discussed: — standard as a bolus 1 mg every 3-5 min in solutions 1:1000 or 1:10000; — average as a bolus 2-5 mg every 3-5 min.; — incremental as a bolus 1—^3 —'5 mg in 3 minutes; — high as a bolus 0.1 mg/kg every 3-5 min. K. Grower and D. Cavallaro (1996) suggest if the effect of standard dose is absent to introduce it once again in 3-5 min., and then to increase the dose fast up to 3-5 and 10-15 mg, whereupon to change over to an infusion at the rate of 100-200 mg/min. The infusion may be started without a preliminary administration of high doses as a bolus. A survival rate increase as a result of high doses has not yet proved, though there is no harm from them in case of circulatory arrest. Atropine may be considered as the other preparation of "primary administration" that is introduced either just after adrenalin injection or after appearance of independent cardiac contractions. It blocks a vagal action inhibiting sinoatrial and atrioventricular nodes. It is administered as a bolus 2-3 times in the course of resuscitation in the doses of 1 mg - 0.5 - 0.5 mg not exceeding a total dose of 2 mg. A need to administer sodium bicarbonate is controversial, but if it is still decided to administer, then do it only after carrying out generally accepted measures (APV, a closed-chest cardiac massage, defibrillation, tracheal intubation), no earlier than 10 min from the onset of resuscitation, starting with 1 mmol/kg and repeating a half dose every 10 min., and better under the control of arterial blood gases. A way of administration is only intravenous, introduction into the trachea is dangerous because of the inhibition of ciliary epithelium activity. The application of sodium bicarbonate in the course of resuscitation may be accompanied by undesirable effects: a growth of intracellular acidosis because of the increase of carbon dioxide content, a shift of oxyhemoglobin dissociation curve to the left, catecholamine inactivation, decrease of the efficiency of defibrillation. Some authors recommend to use 120 mg of lidocaine intravenously as a jet with subsequent continuation of the same dose administered drop by drop. However, there are some data that decreasing the risk of fibrillation lidocaine increases the risk of asystolia development. It is expedient to apply lidocaine in fibrillation refractory to defibrillation. Administration of 10.0 ml 10% calcium chloride is possible in cardiac arrest on the background of preceding hyperkaliemia, hypocalcemia and overdosage of calcium channel blockers. In the rest of cases the use of calcium chloride is doubtful since it may cause development of myocardial contracture or so-called "stone heart". ECG-diagnosis is carried out with a purpose to determine one of three types of circulatory arrest — electromechanical dissociation, ventricular fibrillation or asystolia. In order to do this in urgent situation, only one standard lead is usually sufficient: in asthenics and normosthenics — II, for hypersthenics — III. In order not to interfere with cardiac massage and defibrillation, it is convenient to apply ECG electrodes on the extremities or to use defibrillator electrodes, if it is stipulated by its construction. Electromechanical dissociation (EMD) (or ineffective heart, or agonal ventricular complexes) may be the result of: — "dry" heart when the inflow of blood to the heart is significantly diminished; — "blocks of pulmonary circuit " when the blood from the right chambers of the heart do not enter the left ones; — "cardiac weakness" when a myocardial contractility is sharply decreased. elimination of its cause: critical hypovolemia (infusion of crystalloids and colloids), cardiac tamponade (paracentesis of the pericardium), strained pneumothorax (a change-over to an open pneumothorax or drainage of pleural cavity with continuous aspiration), circulatory collapse (vasopressors), TEPA (thrombolysis), acute cardiac failure (cardiotonics — adrenalin, dopamin, dobutrex). Ventricular fibrillation — is a prognostically favorable type of circulatory arrest since electrical activity of myocardiocytes and contractility of separate fibers contracting asynchronously are preserved. It may be caused by: — acute myocardial infarction; — myocardial ischemia; — Ill degree atrioventricular block; — cardiomyopathies; — intoxication with digitalis preparations; — hypoxia; — acidosis; — electrolyte disbalance;
— contusion or injury of the heart; — electric current injury; — intoxication with narcotics. The most effective method of restoration of synchronous contraction of myocardiocytes (systole) is electrodefibrillation. An absolute indication for its carrying out is the availability of ECG-signs of ventricular fibrillation, however, it is indicated even in case of impossibility to differentiate the type of circulatory arrest taking into consideration a high rate of fibrillation as the cause of the arrest. Before carrying out a defibrillation adrenalin is administered that contributes to the transition of fibrillation to a macrowave one, the latter yields easier to defibrillation. Proceeding from aforesaid, in each circulatory arrest, even having not convinced whether a fibrillation is present or not, one should perform defibrillation just after adrenalin administration. If there is no effect from defibrillation, it is necessary to continue a cardiac massage, to repeat administration of pharmacologic agents and to conduct a second defibrillation. In practice an appearance of independent cardiac contractions took place after the 50-th discharge of the defibrillator. Reference values of voltage, applied in the beginning of defibrillation, are given in Table 5. Table 5 Reference values of voltage of electric current for defibrillation
c V In repeated defibrillation voltage is increased by 500 volts, but no more (than 7000 volts. Since foreign defibrillators generate monopolar impulses of electric current, and domestically produced ones — bipolar, asymmetrical quasi-sinusoidal Gurvich impulses, recommended quantities of discharges of these types of defibrillators do not coincide (Table 6). Table 6 Quantities of discharges in repeated defibrillations (in accordance with L.V. Usenko et al. 2001)
Outcomes in defibrillation: 1) cardiac beats start, hemodynamics is restored; 2) fibrillation changes over to asystolia. In such cases it is necessary to continue a cardiac massage and administer adrenalin in increased dose. Asystolia is turned into fibrillation and defibrillation is performed again with a discharge 500 V higher than the preceeding one, but no more than 7 kV; 3) a threefold defibrillation is of no effect. In order to increase a sensitivity of the myocardium to electric current lidocain is slowly introduced intravenously 1 mg/kg as a bolus, whereupon defibrillation is repeated decreasing the quantity of the first, after lidocaine, discharge down to 200-250 J (4-5 kV). If this manipulation is of no effect lidocain administration may be continued by 0.5 mg/kg every 5-10 minutes or drop by drop at the rate of 2-4 mg/min. (30-500 mg/kg/min.) with subsequent decrease of the rate in the course of 2 hours. If lidocain is of no effect one should proceed to administration of bretylium tosylate, that like lidocain increases a sensitivity of the myocardium to electric current and decreases the danger of fibrillation recurrence. It is injected intravenously 5 mg/kg with subsequent defibrillation. If the effect is absent the same dose is repeated 2-3 times or it is increased up to 10 mg/kg conducting a defibrillation after each administration of bretylium. When fibrillation is being continued a solution of magnesium sulfate 1-2 g/kg is infused intravenously, leading to a decrease of myocardial conduction and excitability. In absence of defibrillator an attempt of chemical defibrillation can be made for this 5 ml 7.5% KClare introduced intravenously or 1% lidocain solution — 5-10 ml (slowly). This defibrillation is less effective, asystolia arises often after it and one fails to control it with the help of other agents. But in persistent fibrillation they, sometimes, resort to chemical defibrillation in absence of any effect from the electrical one. Technics of defibrillation: Skin is to be degreased, a 4-layered gauze serviette moistened with hypertonic solution or current conducting paste is to be layed under electrodes. Defibrillation is distinguished as transversal and longitudinal. In transversal defibrillation electrodes are arranged as follows: 1-st under the left shoulderblade, 2-nd — along a parasternal line in III—IV intercostal space on the left, and are pressed with a strength of 3-4 kg. The first electrode may be placed under the right shoulderblade, the second one — along a parasternal line to the left in III-IV intercostal space. The effectiveness when the dorsal electrode is arranged under the right shoulderblade is higher. When a defibrillator is used for longitudinal defibrillation one electrode is applied in II intercostal space to the right along a medioclavicular line, the second — on the left along a parasternal line in IV intercostal space. The effectiveness of longitudinal defibrillation is lower than that of transversal, but to use such defibrillator is more convenient. Of the domestically produced defibrillators we use apparatuses DI-03-04 for a transversal defibrillation and DI-1D — for a longitudinal one. There are also other types of defibrillators (for example, a pocket defibrillator) that operate automatically in case of cardiac fibrillation. Asystolia is a type of circulatory arrest that is the most prognostically favorable since it is characterized by a complete absence of electrical activity of cardiomyocytes. For excitation of electrical activity on the background of APV and cardiac massage, adrenalin is administered according to the earlier given scheme and atropine 3 mg intravenously or 6 mg endotracheally, without repeated administrations. If electrical activity does not arise after a three-time administration of adrenalin, medicamentous therapy is supplemented with introduction of sodium bicarbonate as was indicated above. Effect of asystolia treatment may be manifested by a restoration of cardiac activity, but more often — by appearance of fibrillation requiring a proper therapy. Resuscitation measures are continued, at this stage, up to the restoration of blood circulation, then in the special care ward of the hospital where the III stage of CPCR is carried out. Ill stage of CPCR — a protracted maintenance of life — is the treatment of post-reanimation disease, stages G, H, I — grade, human, intensive care (see algorithm of the III stage of CPCR on page 100). The aim: restoration of higher cerebral functions. Estimation of patient's condition, CNS functions, maintenance of WEE and ABB, treatment of complications, are carried out. The estimation of patient's condition after a restoration of blood circulation is conducted in the direction of diagnosis and treatment of the cause of death in order to prevent its recurrence, and for the evaluation of the degree and character of disorders occurred in the organism we apply Glasgow standard coma scales (Table 7) and the scale of traumas (Table 8).
Table 7 Glasgow coma scale (1977)
Categories of depth 1 — 14-15 From 1 to 5 the depth of coma of coma and prognosis 2 — 11-13 increases, and the prognosis 3 — 8-10 becomes more unfavorable. 4 — 5-7 5 — 3^1 Postresuscitation disease (PRD): It is a complex, peculiar pathologic process associated with the period of clinical death, resuscitation and subsequent life after it. Stages of postresuscitation disease (E.S. Zolotokrylina, 1999): I stage (6-8 hours since the beginning of treatment) is the stage of unstable II stage (10-12 hours since the beginning of treatment) is the stage of relative Increase of K+ losses and delay of Na+ are noted in the organism, lactate acidosis, developed earlier, is maintained. Expressed hyperenzymemia is also observed. A fibrinolytic activity of blood plasma is significantly slowed down. Table 8 Scale of trauma (1981)
III stage (the end of the 1 -st - 2-nd days of treatment) is the stage of repeated aggravation of patient's condition. Tachycardia, dyspnea, AP elevation, anxiety are observed among some of them, in persons of young and middle age in particular, while their body temperature is normal. A hypoxia of mixed genesis is formed as a result of maximum decrease of oxygen transport in connection with the disturbances of hemoglobin properties and certain difficulty of oxyhemoglobin dissociation, maintenance of tissues diminished perfusion, shunting of blood flow in the lungs and hypodynamic state of blood circulation. At this stage, disturbances of homeostasis and fibrinolysis are maximally pronounced that creates conditions for the appearance of microthromboses in the organs and tissues. Disorders of functions of parenchymatous organs are developed: kidneys by the type of functional oliguria; growing ARF by the type of nonspecific lesion of the lungs ("shock lung") and more rarely — of the liver. All these disorders bear a functional character and are reversible in case of favorable course. IV stage (the 3-rd - 4-th days) has a dual course: favorable — a period of stabilization and subsequent improvement of disturbed functions with a possibility of decreasing the intensity of treatment and complete recovery without complications; unfavorable — a period of further aggravation of patient's condition in connection with progression of the generalized inflammatory response and disturbances of many functions of the organism.Intensification of catabolism, interstitial pulmonary edema, edema of the brain and subcutaneous fat, a deepening of hypoxia of mixed type and hypercoagultion, appearance of pyoinflammatory complications are also noted. Manifestations of insufficiency in the functions of organs and systems are being developed on this background: secondary hemorrhages from the upper sections of GIT (erosions), psychoses with hallucinatory syndrome, secondary cardiac insufficiency, intensification of APF, pancreatitis, disorders of hepatic function, acalculous cholecystitis. V stage (the 5-th - 7-th days) is observed only in unfavorable course of A postresuscitation disease is inevitably accompanied by posthypoxic encephalopathy — a temporary or persistent disorder of CNS functioning occurring as a result of the acute total hypoxia of cerebral cells. The course of this principle pathogenetic component of the postresuscitation disease proceeds in two phases: I — acute phase (catabolic) lasts 2-3 days: A) an activation of metabolic processes or their inhibition in case of adaptation failure; B) development of energy deficit in neurons; C) endogenic intoxication of intracerebral and extracerebral genesis. II — phase of stabilization: A) unstable stabilization of homeostasis (exertion and exhaustion of adaptive B) stable stabilization of homeostasis lasts from several weeks up to months. extracerebral measures taking into account a stage-by-stage course (in accordance with V.I. Cherny, 1997): A. Measures of intracerebral effect I. Creation of protective inhibition and decrease of energy demands of the 5% sodium thiopental solution (a single dose up to 5 mg/kg) and sodium hydroxy-butyrate (a single dose 20 mg/kg) are administered in subnarcotic doses alternately. Sodium thiopental is introduced in 3 hrs, and sodium oxybutyrate — in 2 hrs. In case of diminution of neurological deficit the intervals between administrations are increased and doses —- diminished. II. Restoration of functions of cell and vascular membranes: 1. Decrease of their permeability (prednisolone 1-4 mg/kg i/m per day, having divided the dose into 3-4 administrations, ascorbic acid 4-12 mg/kg daily), a decrease of activity of callicrein-kinin system and trypsinemia, a decrease of enzymemia (contrycal 150-800 U/kg). 2. Decrease of intensity ofLPO (tocopherol 2-8 ml of 30% solution a day, unithiol by 5 ml i/v and aevitum by 2 ml i/m twice a day). III. Restoration of cerebral circulation: 1. Restoration of microcirculation in the vessels of the brain (euphilline 2. Improvement of venous outflow from the cavity of skull 3. Control of brain edema (mannitol 0.25-0.5 g/kg a day, but glycerol, taking 4. Restoration of volume rate of cerebral blood flow (decrease of intravascular pressure with the help of sermion 4-8 mg i/v or i/m, cavinton 15-30 mg and stugeron 75-150 mg a day). IV Control of ammoniemia (a drop-by-drop administration of 1% glutaminic V Restoration of nerve cells metabolism (pyracetam or nootropil 8-12 g a VI. HBO (10 procedures in the regimen of 1.2-1.5 atm no earlier than 3-4 days later after clinical death). B. Measures of extracerebral influence I. Correction of hypovolemia and disorders of central hemodynamics is carried out in accordance with generally adopted principles with a correction for a need to create a moderate hypervolemic hemodilution. II. Normalization of function of respiration. Treatment of respiratory distress syndrome. Ensuring an adequate patency of respiratory tracts both for the period of coma and after a recovery of consciousness. In absence of spontaneous breathing or in its inadequacy APV is applied. Treatment of respiratory distress syndrome is carried on by the principles given in the appropriate section. III. Correction of disorders of water-electrolyte balance and acid-alkili IV Correction of hemocoagulation system disorders consists of measures V Prevention and treatment of hepatic and renal insufficiency (measures VI. Correction of immunologic reactivity disorders is implemented partially VII. Prevention and treatment ofpyo-septic complications is achieved with VIII. Enteral and parenteral feeding. In order to restore the function of the IX. Detoxication therapy (forced diuresis, ultraviolet irradiation of X. Infusion ofperftoran (according to L.V. Usenko et al., 2001, supplements 2. Delayed prognosis: It is established in the course of the first 24 hours. — favorable — a depth of coma decreases, absence of convulsions and decerebrate rigidity; — grave — absence of spontaneous breathing and corneal reflexes for more than 4 hours, dilated and deformed pupils, persistent anisocoria, absence of light response, hypertension of extensor muscles, convulsions; — hopeless — rhythmic myoclonias on the background of coma. Table 9 Scheme of perftoran prescription in PRD
* Infusion is carried out with the aim to prevent development of ischemic and reperfusion syndrome. ** A repeated infusion is prescribed in case of need to control a mixed hypoxia and the secondary ischemia of the brain. In order to increase the effect of perftoran infusion it is recommended to combine it with oxygen inhalation (40-60%) for the period of 24 hours since the beginning of infusion. PROGNOSIS FOR PRD: /. Early: — if a circulatory arrest is less than 4 minutes — prognosis is relatively favorable; — more than 7 minutes — prognosis is extremely doubtful; — it is hopeless in circulatory arrest for more than 20 minutes. If duration of circulatory arrest is unknown, the prognosis is being built on the restoration of reflexes and respiration: — respiration was restored no later than in 20 minutes, a favorable outcome Based on the EEG: — it was normalized in 10 minutes — prognosis is favorable; — in 30 minutes — a favorable outcome is possible; — in more than 30 minutes — an outcome is unfavorable. Дата добавления: 2015-02-05 | Просмотры: 1063 | Нарушение авторских прав |
 Fig. 26. Esophageal obturator
Fig. 26. Esophageal obturator