|
|
АкушерствоАнатомияАнестезиологияВакцинопрофилактикаВалеологияВетеринарияГигиенаЗаболеванияИммунологияКардиологияНеврологияНефрологияОнкологияОториноларингологияОфтальмологияПаразитологияПедиатрияПервая помощьПсихиатрияПульмонологияРеанимацияРевматологияСтоматологияТерапияТоксикологияТравматологияУрологияФармакологияФармацевтикаФизиотерапияФтизиатрияХирургияЭндокринологияЭпидемиология |
LIST OF REFERENCES. Albert A.Selective toxicity: physico-chemical bases of therapy: in 2 volumes
Albert A. Selective toxicity: physico-chemical bases of therapy: in 2 volumes. - M.: Medicine, 1989. - P.400, 432. Alexandrov D., Vyshnatskaya-Alexandrov V. Emergency medical care in internal diseases. - Warsaw: Polish medical publishing house, 1979. - P. 204-225. Bunyatyan A.A., Ryabov G.A., Manevich A.Z. Anesthesiology and reanimatology. - M.: Medicine, 1984. - P.425-433. Chepky L.P., Zhalko-Titarenko V.F. Anesthesiology and reanimatology. -Kiev: Vysshaya shkola, 1983. - P.327-337. Extreme and medical medicine. Collection of test tasks / V.I. Molchanov, Yu.A. Babushkin, V.V. Kudinov et al. / Reviewer O.N. Spitsin; Crimean State Medical University named after S.I. Georgievsky. - Simferopol: Tavrida, 2002.-263 pp. First aid in drug and everyday poisonings / Bobkov Yu.G., Lebedev G.P., Uryupov O.Yu. et al. - L.: Medicine, 1972. - 168 pp. Fundamentals of reanimatology in acute poisonings / Luzhnikov E.A., Dagaev V.N., Firsov N.N. - M.: Medicine, 1977. - 376 pp. Handbook on measures of the first medical aid and prevention of poisonings, injuries and diseases associated with shipment of dangerous cargoes / Ed. by A.A. Lobenko. - Odessa, 1992. - 82 pp. Linden C.H. Diagnosis and Differential Diagnosis of Poisoning // Intensive Care Medicine / Edited by J.M. Rippe, R.S. Irwin, M.P Fink, FB. Cerra. - Vol. I. -Boston - New York - Toronto - London: Little, Brown & Co., 1996. - P. 1478-1487. Linden C.H. General Considerations in the Evaluation and Treatment of Poisoning // Ibid. - P. 1455-1478. Ludevig R., Los K. Acute poisonings. Transl. from German. M.: Medicine, 1983.-560 pp. Luzhnikov E.A. Clinical toxicology. - M.: Medicine, 1982. - 368 pp. Medicine of catastrophes: Teaching aid / Ed. by V.I. Molchanov. -Simferopol: Tavrida, 2002. - 308 pp. Surgical methods of treatment of acute poisonings / Komarov B.D. Luzhnikov E.A., Shimanko I.I. - M.: Medicine, 1981. - 283 pp. Textbook for practical classes on anesthesiology and reanimatology /Ed. by L.V. Usenko. - Kiev: Zdorov'e, 1995. - P.169-232. Teaching and methodical aid on anesthesiology - reanimatology and intensive care of emergency states for students of medical and stomatological faculties, interns, doctors of the faculties of postdiploma education, anesthesiologists-resuscitators. Part II. / Ed. by V.I. Molchanov. - Simferopol, 2000.-105 pp. Vladyka A.S., Lobenko A.A. Poisonings // Handbook for a ship's doctor /Ed. by A.A. Lobenko.-Kiev: Zdorov'e, 1983.-P. 181-192.
3.8. FEATURES OF INTENSIVE CARE IN CHILDREN Carrying out anesthesia and intensive care (IC) requires a knowledge of anatomicophysiologic peculiarities of children's organism. It is necessary to remember a lack of perfection and rapid exhaustion of compensatory mechanisms of respiratory function, thermoregulation and cardiovascular system. A dosage of medicinal agents is made individually taking into account clinico-physiologic data. It is of particular significance for newborns and premature infants since they are the patients with a very high degree of risk. In connection with discrepancy of the rates of development of different systems in the first months of child's life a high consumption of oxygen, excessive heat emission and heat production are noted. Insignificant stores of energy, immaturity of central nervous system and small body mass lead to the fact that under the action of various factors, including IC, a child passes from one critical state to the other. So, in carrying out an infusion therapy dehydration may be replaced by hyperhydration and inadequate oxygenation in hypoxemia leads to hyperoxia. Of all the organs and systems in infants of the early age a nervous system is the least developed. A mass of a child's brain makes up approximately 1/8 (12%) part of the body mass (in adults — 1/40). This is associated with the increased hydrophilic property of tissues. In newborns cerebral gyri are insufficiently expressed. Their differentiation occurs, mainly, under 3 years and only at 8 — is completed. Subcortical sections and blood-brain barrier are insufficiently developed, the latter is more permeable for fluid, medicinal and toxic substances. All this creates some prerequisites for a cerebral edema development even in moderate hyperhydration. In connection with insufficient differentiation of the brain cells a majority of reflexes in newborns is implemented through a subcortex. As a result of this a convulsion syndrome may develop in response to stimuli (pain, hypothermia, dehydration, hyperhydration, some medicaments). Insufficient development of vegetative nervous system often leads to destabilization of respiratory function, blood circulation, thermoregulation and other vitally important functions of the organism. A state of child's hemodynamics at the moment of birth reflects a transitional character between the circulation of fetus and infant. Shunts are preserved between the right and left atria and pulmonary artery and aorta. In connection with this the blood saturated with oxygen flows through the umbilical vein into vena cava inferior, where it is mixed with the blood that outflows from the lower extremities and organs of the abdominal cavity. In time a partially mixed blood comes into the right atrium and through the left ventricle in the aorta. Thus, the greater portion of blood flow of pulmonary artery bypasses the lung, as long as a pulmonary vascular resistance is significantly higher than the systemic one. At the moment of birth, when an umbilical cord is squeezed, a pulmonary circulation increases and the pressure in the left atrium becomes greater than in the right. Under favorable conditions in the course of 2-3 weeks the shunts stop to function, but under the unfavorable ones — a sharp disorder of blood circulation may come on. As a result of acidosis, hypoxemia, hypercapnia and catecholaminemia a vasoconstriction arises. A vascular circulation in the lungs increases and a patent oval foramen and Botallo's duct start again to function: up to 80% of the blood from the cardiac output is discharged through the shunts. Oxygen inhalation and a use of/3-adrenoblockers contribute to a decrease of hypertension in pulmonary circulation and closure of shunts. The weight of the heart in relation to the body weight 1.5 times higher than in adults. By 6-7 month the weight is doubled and to 1.5-2 years — is tripled (very rapid growth), then it slows down and in the period of puberty increases again. Upon birth the right half of the heart is equal to the left one. The volume of the heart increases, from birth to maturity 12 times, and a cardiac beat, under 5-7 years, is defined in the IV intercostal space, and later it may be determined in the V intercostal space interiorly from a papillary muscle, the boundary of dullness of percussion sounds is wider up to 12 years. The first sound is weakened up to 2 years, in addition it is more distinct and stronger that in the adults. The arteries and veins in children are almost of equal width (in adults a lumen of veins is 2 times as much as that of the arteries). In children's organism a cardiac muscle is well supplied with blood since its capillaries are wide. The energy of blood circulation is twice as much as in adults. Child's circulation is under more favorable conditions. At birth a cardiovascular system is maturer than other systems. A large heart and great lumen of vessels facilitate blood circulation, harmful factors such as infection, alcohol and nicotine do not act on cardiac muscle, therefore, it has great reserve potentialities. Pulse in sucklings — 3-3.5 cardiac contractions per 1 respiration, with age it undergoes changes. So, in sucklings it makes up 120-140 beats per min, in the second half of the year— 110-130, by 1-2 years— 110-120, by 3-4 years — 100-110, at 5 years — 100, at 10 years — 78-85, by 13 years — 72-80 and by 15 years — 70-76 beats per min. In children AP is lower than in adults. Under 1 year — a systolic pressure is equal to 80 mm Hg, in time — 80 + number of years x 2. A diastolic AP makes up a half of the systolic one + 10. The blood velocity and the rate of cardiac contractions are significantly higher that is associated with higher metabolism and oxygen "consumption. In sucklings VCB is also relatively increased, in the first months of life it makes up to 10% of body mass, and by 6-7 years it decreases down to 7-8%. At birth VCB makes up, on the average, 350-400 ml, that is why a blood loss of the order of 40-60 ml is significant. Insufficient development of muscular elements in the arterioles and precapillary sphincters, on the background of stress, may lead to the disorder of microcirculation and centralization of blood circulation. Taking into consideration that a significant portion of blood is in the lungs and the heart, a state of shock develops in children more often than in adults. Hemopoiesis in a child is being formed in the embryonal period. In the newborns it occurs in the bone marrow of all bones. Gradually a red marrow is replaced with a yellow bone marrow, and since 12-13 years the blood is generated only in flat bones and in epiphyses of tubular bones. In newborns neutrophilia is noted up to 65%, at 3 years — to 55% of lymphocytes, at 4-5 years the number of neutrophils is equal to the number of lymphocytes, and in school years a neutrophilia is marked again. Imperfection of hemopoiesis often contributes to development of anemia, but in children a relatively high ability for regeneration is noted. Lymph nodes in children are underdeveloped, their growth and development finish prior to 12-13 years. A child has higher hemoglobin content in blood. In the newborns — Hb 110-240 g/1, in sucklings — 110-130 g/1 that contributes to a more effective oxygen transport to the tissues. Along with this, a high hematocrit and presence of fetal hemoglobin in blood worsen rheologic properties of blood. A low hemoglobin content and hyperthermia in septic states increase blood viscosity that may lead to the development of DIC syndrome. Thus, under the unfavorable circumstances an acute cardiovascular failure develops more often in children than in adults. Respiratory tracts of a child have some anatomical features. Their narrowness in the upper sections, absence of teeth, prolonged evacuation of the stomach (up to 8 hours), relatively large tongue, soft and high located epiglottis, narrowness of trachea in the area of cricoid cartilage often lead to a disturbance of the patency of respiratory tract. Owing to the above anatomical interrelations of the tongue, epiglottis and larynx, a direct tracheal intubation is often impeded in children. Small volumes of the anatomical dead space and respiration intensify the danger of a sharp increase of the dead space in resuscitation measures. This volume, for example, is increased in improper use of face mask in oxygen inhalation. Potential chances of development of hypoxic hypoxia in a child are also associated with a thickened alveolar-capillary membrane and underdeveloped respiratory center. As a result of this a diffusion of gases, rhythm and rate of respiration are disturbed. In pulmonary tissue: its elasticity is reduced, a great blood filling and less air inflation are noted. A thoracic cavity is relatively small, respiratory muscles are underdeveloped and they predetermine a limitation of respiratory excursions. A weak development of elastic tissue and limitation of excursions often lead to development of atelectases, particularly in the lower sections of the lungs that are poorly ventilated. With growing age connective tissue elements are replaced by elastic ones, the number of alveoli and VC increase.The lungs are dilated, chiefly, in the direction of compliable diaphragm, therefore, when a child starts to walk his breathing becomes primarily diaphragmatic, later — thoracic and thoracoabdominal. In children pulmonary ventilation does not differ from such in adults. The strength of respiratory muscles is limited. A respiratory surface of the lungs is small and oxygen insufficiency is compensated by the rate of respiration. A child cannot breathe slowly and deeply, therefore, a gas exchange is maintained by hyperventilation. After birth a proper breathing is established only in a few days. The number of respiratory movements in newborns, on the average, is 40-60 per min. With years respiration becomes infrequent and achieves the rhythm of the adult. The age rate of respiratory movements in children is given in Table 30. Table 30 Respiration rate in children
Prior to 8 years in boys respiration is more frequent than in girls. In children a light excitability of the respiratory center is noted. Therefore, even in insignificant physical exercise, psychic excitation, elevation of body temperature and ambient air respiration becomes more frequent. Respiratory volume in newborns, on the average, makes up 20 cm3, in a one-month old infant — 80 cm3, at 5 years — 150 cm3, at 12 years — 250 cm3, at 14-16 years — 300-400 cm3. These values may sharply vary depending on situation. So, for example, if a child cries a volume of respiration increases 2-5 times. Respiratory minute volume in newborns — 800 — 900 cm3, at the age of one month — 1400 cm3, in one-year old — 2600 cm3. Vital capacity depending on the age of the child is given in Table 31. Urogenital system. The kidneys in children are located low, their lobulation disappears by 8 years. The ureters are wide and elastic, with weak muscular layer. In the first 6 months there are 20-25 urinations per 24 hours. At the age of 1 month diuresis are 300 ml, 1 year — 600 ml, 4-5 years — 1000 ml, 10 years — 1.5 1. Table 31 Vital capacity in children
Endocrine system. There are not many hormones in newborns. In the first months thymus gland develops, at the age of 3-4 months — thyroid gland, and a little later — the anterior lobe of the hypophysis. Sexual glands mature by 11-15 years. Gastrointestinal tract.The oral cavity of a child is relatively small. The tongue is large, mucous membrane is delicate, rich in blood vessels, dry and tender. The esophagus is relatively large, the distance from alveolar process to cardial portion of the stomach is 17 cm, at the age of 1 year — 20 cm, at 2 years — 25 cm, at 4 years — 30 cm. A mucous membrane of the esophagus is delicate, rich in vessels, muscular layer is weak. The muscular layer of the stomach is also weak. An empty stomach is shortened, its entrance is wide, therefore, in children vomiting arises rather easily. In one-year old infant the volume of the stomach is 250 ml. The intestine is long (6 body heights, in adults — 4). Muscles are weak. The permeability of the intestinal wall is increased, therefore, a barrier function is reduced for toxins. The innervation of the intestine is imperfect, food passes through it for 12-36 hours. The liver is large. Taking into account that medicaments, in their prolonged application in particular, have a negative effect upon the growing organism, they have to be used in consideration of the dose and age features, as well as functional and pathological disturbances. In order to determine a child's weight of the first year of life one makes use of simple, but very approximate calculation: weight (kg) = weight at birth (3500) + (600 or 500 x number of months of life). The weight of the child after one year (kg) can be approximately calculated by formula: child's weight (kg) = 9.5 + (2 kg x number of years). The child's weight is daily changing, as far as water electrolyte exchange is notable for its dynamic instability. In relation to the body weight the amount of extracellular fluid is twice as much as in adults. With the increase of age its amount decreases achieving the same relative values as in the adults, by 2-3 years of life. Requirement of children's organism in water differs from such in the adults (Table 32). Table 32 A need in water depending on age (by W. Seifart, 1976)
It depends on the higher rate of water exchange and higher water content in children compared to the organism of adults (Table 33). Table 33 Water content in the organism depending on the age (by W. Seifart, 1976)
The absolute amount of blood, plasma and erythrocytes increases simultaneously with a child's body mass. VCB increases with the age (Table 34). Ionic requirements of the children's organism differs significantly from such in the adults (Table 35). Table 34 Body mass, height and VCB depending on the age (by W. Seifart, 1976)
Table 35 Requirement in ions depending on the age
A requirement in Cl~ changes parallel to the changes in Na+ and K+ requirement. AAB in children has also its own features. So, they have a tendency to acidosis. A respiratory regulation of AAB proceeds very rapidly, and renal one, on the contrary, — very slowly. Therefore, while carrying out APV in children one should very carefully select a regimen of ventilation. In infusion therapy a fast introduction of fluid is not recommended, as long as it may lead to acidosis. It is necessary to administer diuretics for children cautiously since a fast loss of liquid may cause alkalosis. Requirements of the child's organism in energy and protein are significantly higher than in the adults and it is associated with the growth and development of children's organism (Table 36). Calculating the requirements in energy one should have in mind that the organism uses only a certain part of it and that it is received from the exchange of various chemical compounds (Table 37).
Table 36 Requirements in energy and protein depending on the age (by W. Seifart, 1976)
Table 37 Energy values of consumed substances in the organism (by W. Seifart, 1976)
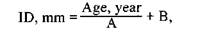
The children of the early age are less sensitive to a decrease of glucose level in blood, hypoglycemia in newborns occurs when glucose concentration decreases down to 2.2 mmol/1. The children of the early age are also very sensitive to a decrease of body temperature. Hypothermia interferes with an oxygen return to tissues, aggravates microcirculation as a result of which metabolic acidosis may develop. On the background of such disturbances an acute cardiovascular insufficiency arises. Hypothermia decreases the enzymatic function of the liver that inhibits hydrolysis of medicaments. In children thermoregulation is inadequate and body temperature is in significant dependence on the temperature of the environment. Therefore, under the conditions of intensive observation a careful thermometry is carried out. A thermostability is insured by the fact that the bed is to be continuously heated to 28-30°C. A hyperthermic reaction also exerts its unfavorable effect on children. It leads to AP decrease, tachycardia, disturbance of the rhythm of cardiac activity. On its background a convulsive syndrome may develop. In hyperthermia physical and medicamenfous means of decreasing the temperature (undressing, bags with ice, wrapping with wet diapers, forced air cooling with a fan On the background of intramuscular and intravenous administration of antipyretics and neuroleptics) are applied. In case of need to perform APV a tracheal intubation in children is to be fulfilled very cautiously, as far as one can easily injure a mucous membrane of the upper respiratory tract. A proper choice of endotracheal tube is of great significance. A choice of the endotracheal gauge is carried out for a concrete patient according to Table 38. For adults and children over 6 years it is recommended to use endotracheal tubes with soft cuffs of large volume that do not traumatize tracheal mucous membranes. For the children under 6 years the tubes without cuffs are applied. In selection of endotracheal tube for children the following formula can be used: Table 38 Gauges of endotracheal tubes depending on the age
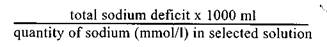
where ID — inner diameter of the tube; A — coefficient equal to 3 for those under 6.5 years and 4 for older than 6.5 years; B — coefficient equal to 3.5 for those under 6.5 years and 4.5 for older than 6.5 years. In carrying out APV during narcosis and operation it is necessary to stick to such rules: — Regimen of moderate ventilation, primarily with a manual method. — Produce a rapid inspiration (2-3 times faster compared to expiration). — A dead space must be minimal. In order to prevent atelectases once in every 10 min a respiratory volume should be increased 3 times. To the peculiarities of carrying out IC in children one must also refer a correction of AAB. A metabolic acidosis is corrected under the control of AAB values with intravenous administration of 4% sodium bicarbonate solution. Along with this an adequate oxygenation may be carried out. In children acidosis may be quickly replaced by alkalosis associated, mainly, with the loss of potassium ions. With the aim of its correction potassium chloride is introduced 2 mmol/kg/day intravenously. It is introduced drop by drop in the concentration not higher than 0.75% in 3% or 10% glucose solution with insulin. A maximal rate of administration should not exceed 1/5 of the daily loss per hour that makes up approximately 3 mmol/1 in the children of early age in the postoperative period. Correction of hyponatremia is carried out by the formula:
Newborns are particularly prone to a loss of sodium. Protein losses in children are replenished with protein containing blood preparations, protein hydrolyzates and amino acid mixtures. The most suitable among them are aminosol, aminol, alvesil, vamin. In severe disorders of protein metabolism a child is administered 3-4 g/kg of protein per day by infusion of blood preparations (albumin, plasma and protein). Children in critical state are to be carried out a wholesome parenteral feeding. On the average, a daily requirement in calories for the children of the first months of life makes up 110 — 130 kcal/kg, for children of 1-3 years — 80-90 kcal/kg, 4-5 years — 70-80 kcal/kg, 10-12 years — 50-60 kcal/kg, at the more senior age — 35-45 kcal/kg. Per every 100 kcal 3-5 mg ascorbic acid, 20-30 mg cocarboxylase, 0.1 mg thyamin, 0.1 mg riboflavin, 0.3 mg pantothenic acid, 5-10 mg choline, 0.7 mg nicotinic acid, 0.1 mg pyridoxine, 2 mg folic acid, 0.04 mg cobalamin are introduced. Parenteral feeding must be balanced. The optimal ratio of proteins, fats and carbohydrates is 1:1.8:6.6. The ratio between the amount of consumed liquid and caloric content of the food makes up 1 ml of water per 1 kcal. At the first opportunity they pass gradually to natural feeding. In pediatric practice a cardiopulmonary and cerebral resuscitation substantially differs from such in the adults. First of all, it refers to the newborns. A depression and asphyxia in newborns may develop quite of a sudden. Nevertheless, before delivery one may anticipate a birth of the child requiring resuscitation, by the availability of antenatal (mother's disease, pathologic pregnancy) or intranatal (complication of the delivery, suppressive effect of medicaments) factors. Waiting for a birth of a child, it is necessary to prepare in the delivery hall some means for suction (rubber balloon, mechanical or electrical suction device, catheters, gastric tube of appropriate sizes), for pulmonary ventilation (a bag insuring 100% oxygen supply, a face mask, nasal airways, oxygen) and intubation (laryngoscope with blades No. 0, 1, endotracheal tubes 2.5; 3.0; 3.5; 4.0, and the guide), as well as medicaments (adrenalin, naloxone, etc.). Succession of resuscitation elements taking into account the time for their carrying out is as follows: In the course of the first 20 sec after infant's birth it is necessary to: — prevent its cooling (radiant heat, wiping the skin dry); — insure a patency of respiratory tract with proper child's position (dorsal or lateral position with the head moderately thrown back) and suction from the mouth and nose; — stimulate breathing (by tapping on the feet, massaging the back) in case of need; — evaluate infant's condition (respiration, HR, color of the skin). If respiration is inadequate — HR is estimated, if no — proceed to pulmonary ventilation. If HR>100 beats per min — evaluate a color of the skin, if less — start a pulmonary ventilation. If a local cyanosis of hands and feet (acrocyanosis) is observed — this is a variant of norm. A central cyanosis of the whole body — it is a manifestation of hypoxemia, the oxygen should be given even in spontaneous breathing. If the oxygen is to be given longer than a few minutes it must be heated and humidified. If meconium appears in amniotic waters there is a probability of its aspiration. The contents of the mouth, pharynx and nose are carefully sucked off, under the control of laryngoscopy — from a hypopharynx, by means of tracheal intubation — from the lower respiratory ways. The indications for carrying out APV: — absence of respiration or breathing of gasping type (to gasp the air); — HR < 100 beats per min. Ventilation is made at the rate of 40-60 times per min and the pressure that produces hardly noticeable elevation and lowering of the chest. Taking in consideration that in the majority of cases one succeeds to ventilate adequately sucklings with the help of mask, it should resort to endotracheal intubation only in case of failure of ventilation with mask. As long as to determine HR in absence of the assistant one has to stop ventilation, in order to reduce waste of time it is counted only for 6 sec. and the result is multiplied by 10. If after 15-30 sec APV with 100% 02 HR < 60 or between 60 and 80 and does not increase, one should start a closed-chest cardiac massage. To carry it out one more participant of resuscitation is needed. Cardiopulmonary resuscitation in children is performed by ABC principle, described in the corresponding section. A feature of a closed-chest cardiac massage in newborns lies in the fact that for the breast bone compression the tips of the middle and second (index) and fourth (ring) fingers of one hand are used. The other hand supports the back of the newborn if he does not lie on a rather hard surface. A massage technique with the thumbs of both hands may be used. In the process, the hands embrace an infant's chest,the thumbs (side by side or one on another) are fixed on the lower third of the breast bone, and the rest — support the back. The breastbone is pressed down for a depth of 2-3 cm. The rate of presses is 90 per min in the ratio with APV 3:1 (90 presses and 30 respirations). HR is determined every 30 sec. If HR achieves 80 and continues to increa se, a massage should be stopped and APV is continued up to the appearance of spontaneous adequate breathing. In case, if a newborn does not response to an adequate ventilation with 100% 02 and a closed-chest cardiac massage, medicaments and blood substitutes are applied in the doses on the basis of body mass that is determined visually before weighing the infant or evaluated prior to the delivery. The way of medicaments administration: — umbilical vein (umbilical catheter); — peripheral veins (hardly accessible veins of the skin of the head and extremities);
— endotracheal instillation. Introduce: — adrenalin 1:10000 0.1-0.3 ml/kg;
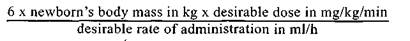
— blood substitutes (in acute hemorrhage with symptoms of hypovolemia) — blood, 5% albumin, physiologic solution, Ringer-lactate solution 10 ml/kg; — sodium hydrocarbonate (in confirmed or probable acidosis) 4.2% slowly for no less than 2 min 2 mmol/kg (4 ml/kg); — naloxon 0.1 mg/kg (0.1 ml/kg solution that contains 1.0 mg per ml). for a use in asphyxia of newborns had not gained evidences of its effectiveness in the acute period of resuscitation. If it lasts a long time and there is a thready pulse in an infant, and other symptoms of shock, to intensify cardiac contractions and to increase AP, after a consultation with a neonatologist, dopamin is administered with a constant infusion with the help of infusor controlling carefully the rate of infusion. They start with the dose of 5 mg/kg/min increasing it, if needed, to 20 mg/kg/ min. For this one makes use of the formula for a calculation of the quantity of dopamin in mg that must be added to each 100ml solution:
For example: — newborn's body mass is 1200 g (1.2 kg); — desirable dose — 5 mg/kg/min; — desirable rate of administration 3 ml/h.
(6*1,2*5)/3= 12 mg dopamin per every 100 ml solution
If resuscitation measures are carried out for the course of the first 4 minutes of asphyxia the prognosis is favorable and no pathologic changes on the part of CNS in these children are not being observed both in the immediate and long-term postresuscitation periods. In asphyxia for the course of 10 minutes normalization of the infant's state occurs on the 8th-10th day, and if for more than 10 min, focal lesions of CNS appear that are accompanied with convulsions and mental disorders. Note that in pediatrical practice as in the adults, intensive care in emergency states requires not only theoretical knowledge, but practical skills as well, mastering which starts on the practical classes and may continue for the whole professional life.
CONTROL QUESTIONS AND TASKS 1. What are the terms of closing the shunts between the right and left atria A. 2-3 weeks B. 5-7 days C. 4-5 weeks D. 2 months E. 3 months 2. In what costal space is a cardiac beat determined in children under i-1 A. IV B. Ill C. II 3. What is HR in sucklings (beats/min)? A. 120-140 B. 150-160 C. 100-110 D. 80-90 E. 60-70 4. What is AP (mm Hg) at the age of 4 according to the formula of A. 76 B. 80 C. 88 D. 96 E. 100 5. What is VCB (ml) in a newborn? A. 100-150 B. 200-250 C. 350-400 D. 500-550 E. 600-650 6. At what age is the number of neutrophils in children equal to the number A. 1-2 years B. 3-4 years C. 4-5 years D. 6-7 years E. 8-10 years 7. What are the values of hemoglobin (g/1) in newborns? A. 0-80 B. 90-100 C. 30-40 D. 50-60 E. 110-240 8. What is the duration of gastric evacuation after taking a meal in sucklings? A. 3 hours B. 5 hours C. 6 hours D. 8 hours E. 12 hours 9. What is the type of respiration in infants prior to walking? A. Diaphragmatic B. Thoracic C. Abdominal D. Thoraco-diaphragmatic E. Thoraco-abdominal 10. What is RR (insp./min) in the 6-year old children? A. 15 B. 20 C. 25 D. 40 E. 60 11. What is RV (cm3) in children at the age of 5? A. 65 B. 75 C. 85 D. 100 E. 150 12. How does RV change in a child's loud crying? A. Decreases 5 times B. Decreases 3 times C. Does not change D. Increases 1.5 time E. Increases 2—5 times. 13. What is RMV (cm3) in infants at the age of 1 month? A. 800 B. 900 C. 1400 D. 2000 E. 2600 14. What is VC (cm3) in the four-year old children? A. 1000 B. 1500 C. 1800 D. 2500 E. 3000 15. What is diuresis (ml) in one-month old infants? A. 100 B. 200 C. 300 D. 400 E. 500 16. What is diuresis in one-year old infants? A. 200 B. 300 C. 400 D. 500 E. 600 17. What is the distance (cm) from the alveolar process to the cardial portion A. 8 B. 10 C. 15 D. 17 E. 20 18. What is the distance (cm) from the alveolar process to the cardial portion A. 15 B. 20 C. 25 D. 30 E. 40 19. What is the volume of the stomach in one-year old infant? A. 50 ml B. 100 ml C. 150 ml D. 250 ml E. 350 ml 20. What must the approximate weight (kg) of the six-month old child be if A. 5.2-4.5 B. 7.1-6.5 C. 8-7.5 D. 9.2-8.5 E. 10-9.5 21. What is the water requirement (g/kg/day) in a newborn? A. 40-50 B. 60-70 C. 80-100 D. 110-130 E. 150-160 22. What is the percentage of water content depending on the newborn's A. 50 B. 60 C. 75 D. 80 E. 85 23. What is the need in Na+ (mmol/kg/day) in a newborn? A. 6-7 B. 3-5 C. 1-2 D. 7-8 E. 9-10 24. What is the need in Na+ (mmol/kg/day) at the age of 12? A. 6-7 B. 3-5 C. 1-2 D. 7-8 E. 9-10 25. What is the need in K+ (mmol/kg/day) in a newborn? A. 6-7 B. 4-5 C. 2-3 D. 7-8 E. 9-10 26. What is the need in K+ (mmol/kg/day) at the age of 12? A. 6 B. 3 C. 1.5 D. 7.5 E. 9 27. What are the energy demands (kcal/kg/day) in a newborn? A. 300-400 B. 200-250 C. 100-120 D. 60-70 E. 40-50 28. What is the protein requirement (g/kg/day) in a newborn? A. 3.5-4 B. 3-2.5 C. 2-1.5 D. 1-0.75 E. 0.5-0.25 29. What is the diameter of the intubation tube (mm) for a four-year old A. 6 B. 5.5 C. 5 D. 4.5 E. 4 30. What is the approximate dose of 4% Na bicarbonate solution (ml/kg) A. 7 B.6 C. 5 D.4 E. 3 31. What is the approximate dose of KC1 (mmol/kg/day) for a correction of A. 7 B. 5 C. 2 D. 1 E. 0.5 32. What gauge (No.) of tubes is necessary for a tracheal intubation of a A. 6-6.5 B. 5-5.5 C. 5-4.5 D. 2.5-4 E. 1-2 33. What of the enumerated below is not the indication for APV of a A. RR 30 respirations per min. B. Absence of respiration C. Gasping type of breathing D. HR 70 beats per min E. HR 40 beats per min 34. For what depth (cm) is the breast bone pressed in a closed-chest cardiac A. 3-4 B. 2-2.5 C. 1-2 D. 5-6 E. 7-8 35. What is the rate of presses on the breastbone (times/min) in cardiac A. 120 B. 110 C. 100 D. 90 E. 80 36. What is the rate of resp./min in APV in newborns? A. 70 B. 60 C. 50 D. 40 E. 30 37. At what minimal spontaneous HR may a cardiac massage be stopped? A. 120 B. 110 C. 100 D. 90 E. 80 38. The wrong way of administration of medicaments in resuscitation of A. Umbilical vein B. Vein of the skin of the head C. Vein of the lower extremities D. Endotracheal E. Intracardial 39. Which of the medicaments is not indicated for administration in A. Adrenalin B. Blood substitutes C. Calcium chloride D. Sodium hydrocarbonate E. Naloxon 40. How many mg of dopamin must be added to 100 ml solution in order to A. 30 B. 40 C. 18 D. 12 E. 10. Дата добавления: 2015-02-05 | Просмотры: 1048 | Нарушение авторских прав |